By using this website, you agree to our privacy policy
×Supporting Maggie's Cancer Charity
We will shortly be publishing a new book called Headstones- Advice and Inspiration and will be selling it to raise money for Maggie's Cancer Charity in Oxford.
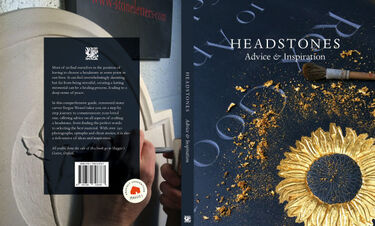
We are really excited to announce that we have nearly completed our new book Headstones- Advice and Inspiration, which we are going to sell to raise money for Maggie's Cancer Charity in Oxford. We will be donating 100% of profits from the sale of the book to Maggie's and the idea for the book came about after my mother died from cancer two years ago.
Maggie’s is an incredible charity that has centres all over the UK, based at hospitals, where anyone affected by cancer can walk in and find a sanctuary and support, away from the clinical environment of the hospital.
Although I’ve visited Maggie’s and heard so many amazing things about the charity, I wanted to get an insider’s perspective. I was thus delighted to meet with Elaine Russell-Jarvie, who worked as a volunteer counsellor at Maggie’s, Oxford for two years between 2017 and 2019.
Reflections on my time at Maggie’s- an interview with Elaine Russell-Jarvie

Here is a transcript of the interview with my words in bold:
What is your background and how did you end up at Maggie’s?
Well, I’d worked for fifteen years for Cruse Bereavement Care in York and had done continual training with them over those years and worked in 1:1 counselling, and I initially planned to continue with cruse and carry on with private work. But then I thought I might like a change and one day I took a friend from the village to an appointment at the Churchchill Hospital on a journey of radiotherapy and I thought I might go and have a coffee at Maggie’s- I was looking out for a place I could take my skills and experience on a voluntary basis part-time so I walked into Maggie’s and I immediately felt the absolute opposite environment to that of the hospital.
Yes, it’s like an antidote.
Yes, a complete contrast to the clinical atmosphere. And later on, as I sat in Maggie’s in the counselling room, I would reflect on the stories going on in this vast building of the hospital, the wonderful work they were doing, hundreds of stories, and how to come across to Maggie’s was such a contrast.
But on that morning, I first went in I got chatting to the manager Claire and I told her I was looking for a place to bring my skills. She grabbed my hand and said “Yes please and as a result of that I found myself there. I agreed to go once a week initially and to take on up to five clients a day. I then cut it down to once fortnightly after a year as the journey was quite arduous and seeing five clients was quite a lot.
And did you always see the same clients?
Yes, I would see them for as long as they required. Fortunately, at Maggie’s it’s open-ended, unlike the NHS where you get offered six sessions, I saw one or two clients for very much longer than that and some as in every situation, some people only needed to come on a one-off basis and offload.
What sort of people tend to come not Maggie’s? All ages, all patients, or families as well?
A lot of families and family members.
So not just the patients?
Yes, the extended family too. I’d say the majority were patients, but we certainly saw husbands, wives, brothers, sisters, daughters, sons, any member of the family who was struggling with the emotional impact.
Is it always people suffering from cancer? The biggest thing must be the fear of death?
Yes, but what surprised me during my time was that there was an awful lot of women in particular who had gone through the process of diagnosis and treatment and come out at the other end where the consultant oncologist gave them the all-clear, and they could go and would just need to be seen every year or six months. And they had stoically and with great courage got their heads down and got through this process, just getting on with it, and then at the end of it, they felt they were on their own. And I would say that often resulted in a kind of post-traumatic stress, when they had been so together and brave, dealing with their emotions and the fear, a real fear that actually “I have a bit of a pain” and “I’m not sure” and real uncertainty about the future.
The other thing I learned was that families, particularly husbands, wives, sons, daughters, would be celebrating, of course at the end of the treatment, celebrating that mum was “ok”. What I hadn’t realised and learned was that recovery takes a long time and just because you are dismissed from the hospital it can take a year or so to recover because you have taken a hammering in so many ways, that you can’t just step back into life as it was. It takes a lot of rebuilding and it’s a slow process and people aren’t necessarily prepared for that. Patients don’t always want to say to their husbands and wives “I’m really quite tired” because the general perception is that they are ok now.
They feel they have to try to be strong
Yes, to be strong and not talk too much about how they are really feeling because everyone around them is so thrilled they are ok and have come through it, and that can be quite difficult because patients want to put on a “back to normal” face but actually it takes a long, long time.
How interesting.
So, in that case, my feeling was that it was useful to talk about the small steps, talk about honesty and communication, talk about accepting support, as often friends do offer and you say “I’m fine”. It’s quite hard to accept support.
Do husbands come in themselves?
Occasionally they do
The other half must also have to deal with a lot and don’t always get the support they need.
Absolutely, and there have been situations when I’ve seen husbands and wives together when really bad news has been given and they are desperately trying to support the other and occasionally people come out from the hospital into Maggie’s in a state of real turmoil and need a place just to find some peace to try and come to terms with what they’ve been told. So there is the other side where yes, I did see a lot of women and men post-treatment, but then we have to also mention that we see people in the midst of real trauma, trying to come to terms with a situation that isn’t going to resolve itself.
How can you help someone who has terrible news? What tools can you give them?
It’s more about allowing them to “be” really and being alongside. Listening. And really, I think that is when a counsellor who is able to exude that sense of caring is so important. Being alongside them in a genuine way. It’s so difficult. That’s about it really.
Can people just walk in unannounced and see someone?
Yes, they do, and they will be met by volunteers who are welcoming and give them a cup of tea and then if they want to talk to somebody, they will be met by one of the front-line cancer specialists. They all have a really strong background in care and know their stuff (medically). So people can ask questions and talk, and the specialists are multiskilled and empathetic in that they have the clinical background but also the ability to listen. If it is felt at that point that specialist 1:1 care is needed in the form of counselling, if they really are clearly struggling in some way in that regard, then one of the specialists will ask if the person would like to see one of their 1:1 counsellors and some notes will be taken and they will be referred. That is how they get to see a counsellor. So if they walk in straight from the hospital, they won’t see a counsellor straight away but one of the cancer specialists will certainly spend time with them and allow them to take their time to talk before referring on to us.
Do the NHS offer counselling or is there a waiting list?
There is a long waiting list, I think. I noticed there might be a strengthening of ties between the hospital and Maggie’s; I’m quite sure that most of the staff at the hospital will know to point people to Maggie’s when they think it will help.
It must be a great help to the hospital staff then.
Yes, absolutely.
So in terms of other agencies that people are signposted to, I’m not sure, but that’s how it works at Maggie’s- people will be seen as soon as they walk in and given time by a front-line specialist staff.
Sometimes people walk in and they will be in turmoil about their finances and there is a specialist at Maggie’s who deals solely with that, and an appointment can be made, and the situation explained and he or she is absolutely up to speed on what financial assistance might be available and how to go about getting it. So that is a really practical way Maggie’s supports people.
Other people might walk in just needing some space and quiet.
Yes, it doesn’t feel clinical at all.
No, it doesn’t feel clinical. There is a warm log burner in the room. The place is full of art and softness and warmth and peace and you can go there, and they offer a range of workshops on relaxation, how to tie headscarves and even will making. All sorts of things from art and singing, all kinds of activities that you can sign up for and go to as well. So it is a real holistic approach. You can get information on the cancer you have. And it may be that someone has just been in front of their oncologist and the information has been too much to understand.
So the nurses can help with that?
Yes and there is lots of information, and a library full of books, and every leaflet you could think of, but all the “nurses” in Maggie’s have had a real solid background in cancer treatment so they know what they are talking about. Although they would never profess to take the place of the patient’s oncologist, they have solid background knowledge and understanding of the conditions.
Are there opportunities to meet other patients too?
Yes, there is always in every Maggie’s in the country what we call the Kitchen Table, and it’s just that; a big table where people can sit around and have a coffee… there’s always cakes and fruit, something to eat.
Is it all free of charge too?
Absolutely yes, and it’s round that table with other patients, relatives, volunteers, and trained staff, that people can sit and often talk in a really informal and supportive place.
So they can share their stories, so they don’t feel so alone? It must be such an isolated feeling
Absolutely, and that is also where the workshops come in, as people gather together for relaxation classes and so on and they meet and make friends at these classes and can share their stories.
So there is a real range of support all within this lovely setting.
So you must have helped so many people over a year? There must be so many people coming in.
Yes, I’d go in and look at my diary which was filled in for me.
It’s a great model- I don’t know of anything like it.
Being at the hospital must be a really important part of it.
Yes, as it’s so accessible.
Maggie’s can be there just when someone needs them most.
Absolutely, and sometimes my clients would try to coincide their clinical appointment to be followed up with an appointment to see me, and that would be really useful. Yes, we see teenagers and young and older adults. Certainly, we see young people who either were patients themselves or their parents or siblings have been patients.
Do you sometimes get a whole family coming?
Yes, the support is there for anyone affected by cancer.
What about after someone has died, do you get the bereaved relatives coming back?
Yes indeed, bereavement support is available and that is where the fifteen years’ experience of mine as a bereavement counsellor was useful for me. Because dealing with people affected by cancer was initially new for me, I didn’t have a background with these cases, but the skills, I was a member of the BACP (British association of counselling and psychotherapy), I’d done three years at university and I was a trained counsellor.
I guess the bereaved come back to you because they have got to know Maggie’s during the treatment of their loved one, rather than having to start from scratch with a new counsellor.
Absolutely, it becomes a safe welcoming place where they know the familiar faces, Maggie’s is somewhere they feel comfortable and relaxed.
Another thing I wanted to mention; one of the things I learned was that the way in which women in particular but also men, how they lose their identity. This was a major issue for them. Perhaps losing their hair, losing the way they looked, they felt quite lost really.
Yes, I can imagine that.
They felt they’d lost themselves and the way other people perceived them changed. The way people reacted to their diagnosis was a big issue and not one I fully understood.
Do people avoid them or not mention it?
The patients seem to lose their sense of self and other people although well-meaning, don’t see them in quite the same way as before because they have cancer, and they may look different. Although I knew that before, I hadn’t realised how profoundly and deeply that can affect women. It’s almost as if they have somehow lost themselves along the way.
Finding themselves again and transitioning back again must also be hard.
Yes.
There were some really good outcomes though at Maggie’s. it was a real reward and could be quite uplifting. A lot came out during sessions. It wasn’t all about the treatment and the disease. I found that often other issues arose and sometimes they brought up issues like abuse, and all sorts of issues came up, so have to be really routed to be alongside people, it wasn’t always about the disease itself.
Yes, people must have been very vulnerable.
That’s when it’s important that people knew that we would be there alongside them whatever the outcome for as long as they needed.
So you must have seen some happy outcomes too.
Absolutely and for some people I had to give people lots of warning before I left Maggie’s.
How long did you see people sometimes?
Sometimes I saw people for several months. We see people for as long as they need us. One particular lady came through her treatment and was beginning to try to pick up the pieces of her life and doing some part-time work, but the cancer gave her the opportunity, this massive event in her life (unwelcome as it was) to really assess and reflect on what she wanted from her life. And this sometimes happened. She started to look at the rest of her life very carefully and decide what it was she wanted to go forward with and what she wanted to leave behind, so it gave her the chance to think in real detail about how she wanted the rest of her life to look. It was a really positive side of her illness. A real journey for her over maybe six months where it gave her a chance to reflect on the things in her life that had brought her to this point and decisions she may have made that were in part due to things that had happened in her relationships with her family members, and it gave her the chance to really think about what is important, so for her, it was really cathartic and she came through the treatment, regaining her health and she had a good part of her life ahead to look forward to and she wanted it to be very much more on her own terms.
So that was really positive and it was a real privilege to walk with her through that process.
Your being by her side must have been really helpful.
Yes, she really appreciated the time and space that I was able to give her.
The continuity must be important, something you don’t always get in the hospital.
Yes, we always see the same person and we always left it up to them to decide how long they needed to come to us. As experienced professional, you can get a sense of when they might need you and you review things regularly, but you get a sense of when the work we are doing is coming to an end. So endings are important. But you need to plan them carefully.
It must be quite emotional saying goodbye.
Yes, it is one of the hardest parts of the work, because you walk with someone through a journey and then our work is done. Maggie’s is there for them always, but our work is done. That’s important, to be able to recognise when the end of our counselling sessions is coming for us and to plan it so that it is gradual. And often the client may be relieved that you’ve noticed. It’s important that they don’t also come for you.
Yes, I can see that. It must be really emotional at times.
It’s incredible work you’ve done. I’m really glad we chose to support Maggie’s. It is incredible how many of our clients have heard of Maggie’s all over the UK.
Yes, Maggie’s Centres are all over the country and also spreading overseas.
I had never heard of Maggie’s when I walked into the Centre that very first day, but I got an immediate sense of something special.
The first centre was set up by Maggie Keswick Jencks who was herself an architect and quite early in her marriage, she was diagnosed with breast cancer and found herself in some draughty dark corridor with her husband having been given the news in a state of shock, and she thought “there has to be a better way, there has to be a better way than this” and so she went away with that idea and began to formulate the concept of Maggie’s where the space is so important, and as an architect, she believed in the ability of buildings to uplift people. There are now nineteen Maggie’s Centres across the UK and abroad and there are plans to open more.
Thank you, Elaine, for sharing with us your experience, it has been really emotional and fascinating to hear your stories.
You are very welcome. I feel very privileged to have been part of Maggie’s.
Conversation between Hannah Wessel (in bold) and Elaine Russell-Jarvie, February 2020
For more information about our new book please sign up to our blog.

Fergus Wessel
Designer and letter-carver
Fergus created Stoneletters Studio in 2003, after training at the Kindersley Workshop. He is a member of the prestigious Master Carver's Association.

Request our free booklet today
- © 2026 Stoneletters
- Legal notice
- Privacy policy
- Disclaimer